Diseases & Conditions
Calcaneus (Heel Bone) Fractures
A fracture of the calcaneus, or heel bone, can be a painful and disabling injury. This type of fracture commonly occurs during a high-energy event — such as a car crash or a fall from a ladder — when the heel is crushed under the weight of the body. When this occurs, the heel can widen, shorten, and become deformed.
Calcaneus fractures can be quite severe. Treatment often involves surgery to reconstruct the normal anatomy of the heel and restore mobility so that patients can return to normal activity. But even with appropriate treatment, some fractures may result in long-term complications, such as pain, swelling, loss of motion, and arthritis. Many patients with labor-intensive jobs are unable to return to their job after a calcaneus fracture.
Anatomy
The bones of the feet are commonly divided into three parts:
- The hindfoot
- The midfoot
- The forefoot
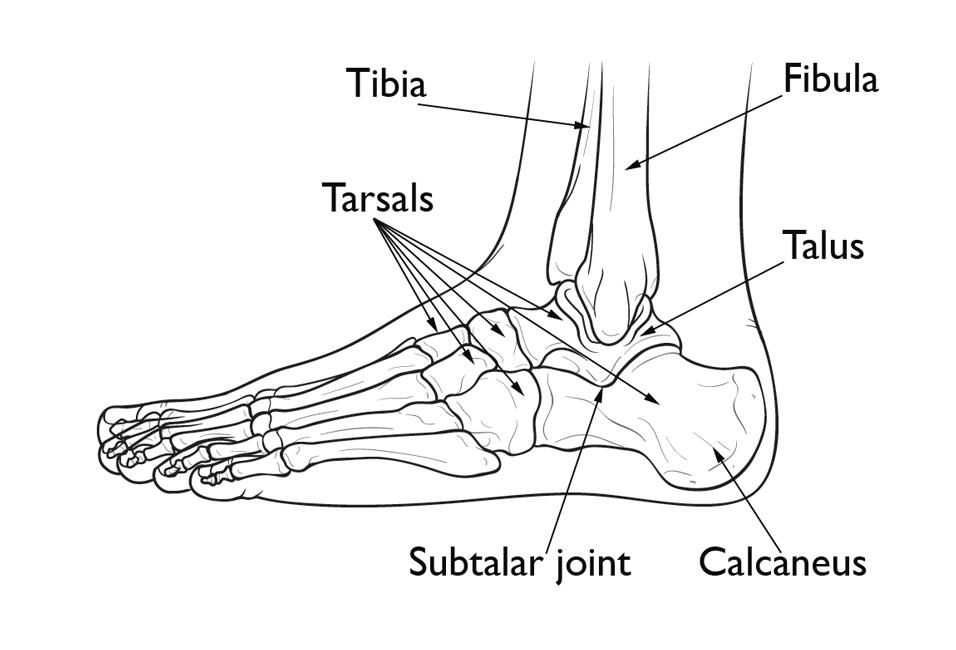
Seven bones — called tarsals — make up the hindfoot and midfoot. The calcaneus (heel bone) is the largest of the tarsal bones in the foot. It lies at the back of the foot (hindfoot) below the three bones that make up the ankle joint. These three bones are the:
- Tibia (shinbone)
- Fibula (smaller bone in the lower leg)
- Talus (small foot bone that works as a hinge between the tibia and the fibula)
Together, the calcaneus and the talus form the subtalar joint. The subtalar joint allows side-to-side movement of the hindfoot and is especially important for balance on uneven surfaces.
Description
Calcaneus fractures are uncommon. Fractures of the tarsal bones account for only about 2% of all adult fractures, and only half of tarsal fractures are calcaneus fractures.
A fracture may cause the heel bone to widen and shorten. In most cases, a fracture also enters the subtalar joint in the foot. When this occurs, damage to the articular cartilage covering the joint may cause long-term complications such as chronic pain, arthritis, and loss of motion.
Severity
The severity of a calcaneus injury depends on several factors, including:
- The number of fractures.
- The amount and size of the broken bone fragments.
- The amount each piece is out of place (displaced). In some cases, the broken ends of bones line up almost correctly; in more severe fractures, there may be a large gap between the broken pieces, or the fragments may overlap each other
- The injury to the cartilage surfaces in the subtalar joint.
- The injury to surrounding soft tissues, such as muscle, tendons, and skin.
When the bone breaks and fragments stick out through the skin or if a wound penetrates down to the bone, the fracture is called an open fracture.
An open fracture often causes more damage to the surrounding muscles, tendons, and ligaments and takes a longer time to heal. Open fractures have a higher risk of infection in both the wound and the bone. Immediate treatment to clean the wound is required to prevent infection.
Cause
The calcaneus is most often fractured during a fall from a height or a motor vehicle collision.
The severity of a fracture can vary, although most are caused by a violent impact. For example, a simple twist of the ankle may result in a single crack in the bone. The force of a head-on car collision, however, may result in the bone being shattered (comminuted fracture).
Similar fractures can result from different mechanisms. For example:
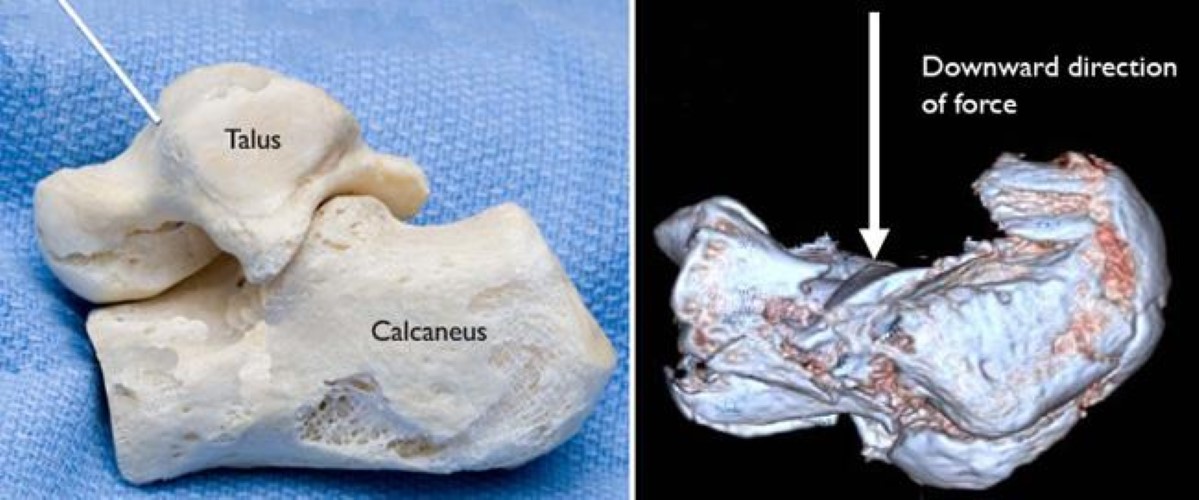
- If you land on your feet from a fall, your body's weight is directed downward. This drives the talus bone directly into the calcaneus.
- In a motor vehicle crash, the calcaneus is driven up against the talus if the heel is crushed against the floorboard.
In both cases, the fracture patterns are similar. As a rule, the greater the impact, the more the calcaneus is damaged.
In a high-energy fracture, other injuries, such as fractures of the spine, hip, or other heel, can occur.
Symptoms
Patients with calcaneus fractures usually experience:
- Pain
- Bruising
- Swelling
- Heel deformity
- Inability to put weight on the heel or walk
With some minor calcaneus fractures, the pain may not be enough to prevent you from walking — but you may limp. This is because your Achilles tendon acts through the calcaneus to support your body weight. If, however, your calcaneus is deformed by the injury, your muscle and tendon cannot generate enough power to support your weight. Your foot and ankle will feel unstable, and you will walk differently.
Doctor Examination
It is important that you tell your doctor the circumstances of your injury. For example, if you fell from a ladder, how far did you fall, and what type of surface did you land on?
It is also important that you tell your doctor if you have any other injuries or medical problems, such as diabetes, or if you take medications or smoke.
Physical Examination
After discussing your symptoms and medical history, your doctor will perform a careful examination. They will:
- Examine your foot and ankle to see if your skin was damaged or punctured from the injury.
- Check your pulse at key points of the foot to be sure that there is a good blood supply to the foot and toes.
- Check to see if you can move your toes and can feel things on the bottom of your foot.
- Determine whether you have injured any other areas of your body by examining the rest of your injured leg, as well as your other leg, pelvis, and spine.
Tests
Imaging studies will help confirm the diagnosis of a calcaneus fracture:
X-rays. X-rays, the most common and widely available diagnostic imaging technique, create images of dense structures, such as bone. An X-ray can show whether your calcaneus is broken and whether the bones are displaced.
Computed tomography (CT) scans. Because of the complex anatomy of the calcaneus, a CT scan is routinely ordered after a fracture has been diagnosed on X-ray. A CT scan will produce a more detailed image of your foot than an X-ray and can provide your doctor with valuable information about the severity of your fracture. This information will help your doctor recommend the best plan for treatment.
Your doctor may share both your X-rays and CT scans with you to help you better understand the nature and severity of your injury.
Treatment
Your doctor will consider several factors in planning your treatment, including:
- The cause of your injury
- Your overall health
- The severity of your injury
- The extent of soft tissue damage
Because most calcaneus fractures cause the bone to widen and shorten, the goal of treatment is to restore the normal anatomy of the heel. In general, patients whose normal heel anatomy is restored have better outcomes, and in most cases, recreating the normal heel anatomy involves surgery. Your doctor will discuss the different treatment options with you.
Nonsurgical Treatment
Your doctor may recommend nonsurgical treatment if the pieces of broken bone have not been displaced by the force of the injury.
Immobilization. A cast, splint, or brace will hold the bones in your foot in proper position while they heal. You may have to wear a cast for 6 to 8 weeks — or possibly longer. During this time, you will not be able to put any weight on your foot until the bone is completely healed.
Surgical Treatment
If the bones have shifted out of place (displaced), your doctor may recommend surgery.
Surgery to repair a calcaneus fracture can restore the normal shape of the bone but is sometimes associated with complications, such as wound healing problems, infection, and nerve damage.
Nonsurgical treatment of some fractures, however, can also lead to long-term complications, such as pain, arthritis, and a limp. Your doctor will review the details of your injury and talk with you about the risks and benefits of surgical versus nonsurgical treatment.
Timing of surgery. If the skin around your fracture has not been broken, your doctor may recommend waiting until swelling has gone down before having surgery. Elevating your leg and keeping it immobilized for several days will decrease swelling. It will also give injured skin a chance to recover. Waiting before the operation may improve your overall recovery from surgery and decrease your risk of infection.
Open fractures, however, expose the fracture site to the environment — increasing the risk of infection — and must be treated immediately. They require surgery to clean the wound and remove damaged tissue.
Early surgery may also be recommended for other fractures. Although uncommon, a piece of the calcaneus can be pulled off when the Achilles tendon splits away from the bone (avulsion). For this type of fracture, emergent surgery can decrease the risk of injury to the skin around the Achilles tendon.
Surgical procedure. The following procedures are used for various types of calcaneus fractures:
- Percutaneous screw fixation. If the bone pieces are large, they can sometimes be moved back into place without making a large incision. Special screws are then inserted through small incisions to hold the fracture together.
- Open reduction and internal fixation. During this operation, an open incision is made to reposition (reduce) the bones into their normal alignment. They are held together with wires or metal plates and screws.
Bones have a remarkable capacity to heal. The more severe your injury, however, the longer your recovery may be. Patients with more severe fractures are also more likely to suffer some degree of permanent loss of function, regardless of treatment.
Pain Management
After surgery, you will feel some pain. This is a natural part of the healing process. Your doctor and nurses will work to reduce your pain, which can help you recover from surgery faster.
Medications are often prescribed for short-term pain relief after surgery. Many types of medicines are available to help manage pain, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and local anesthetics. Your doctor may use a combination of these medications to improve pain relief, as well as minimize the need for opioids.
Be aware that although opioids help relieve pain after surgery, they are narcotics and can be addictive. Opioid dependency and overdose have become critical public health issues in the U.S. It is important to use opioids only as directed by your doctor and to stop taking them as soon as your pain begins to improve. Talk to your doctor if your pain has not begun to improve within a few days of your surgery.
Rehabilitation
Whether your treatment is surgical or nonsurgical, your rehabilitation will be very similar. The time it takes to return to daily activities will vary depending on the type and severity of the fracture and whether you have other injuries.
Some patients can begin weightbearing activities a few weeks after injury or surgery; most will need to wait 3 months before putting weight on the heel. Some patients are able to begin partial weightbearing 6 to 10 weeks after injury or surgery.
- Early motion. Many doctors encourage motion of the foot and ankle early in the recovery period. For example, you may be instructed to begin moving the affected area as soon as your pain allows. If you have had surgery, you may be instructed to begin moving the affected area as soon as the wound heals to your doctor's satisfaction.
- Physical therapy. Specific exercises can help improve the range of motion in your foot and ankle, and strengthen supporting muscles. Although they are often painful at the beginning and progress may be difficult, exercises are required in order for you to resume normal activities.
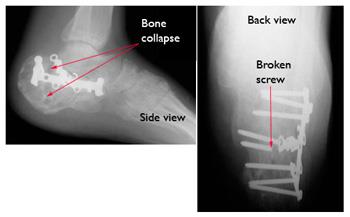
- Weightbearing. When you begin walking, you may need to use crutches, a cane, or a walker and/or wear a special boot. It is very important to follow your doctor's instructions for walking on your foot. If you put weight on your foot too soon, the bone pieces may move out of place and you might require surgery. If you have had surgery, the screws might loosen or break and the bone may collapse. This may not occur the first time you walk on it, but if the bone is not healed and you continue to bear weight, the metal will eventually break.
Complications
Complications often occur with calcaneus fractures. Minor complications include:
- Small or temporary areas of delayed wound healing
- Nerve irritation around the incision
- Tendon irritation
- Joint stiffness
- Chronic pain
- Chronic swelling
Major complications include:
- Failure of the wound to heal
- Infection
- Posttraumatic arthritis (with or without surgery)
It is important to tell your doctor if you are a smoker. Smoking affects both bone and wound healing. With or without surgery, your bone may take longer to heal if you smoke.
Learn more: Smoking and Musculoskeletal Health
Learn more: Surgery and Smoking
Additional surgery is usually required in cases of infection or wound healing complications. If all attempts to resolve an infection or a wound healing complication fail, an amputation may be necessary.
Outcomes
If your injury is minor, such as a crack in the bone with little muscle damage, you may be able to resume normal activities 3 to 4 months after surgery. If your fracture is severe, however, it may take 1 to 2 years before recovery is complete.
Despite the best efforts of the doctor and patient, patients rarely regain normal foot and ankle motion after a severe fracture and do not typically resume their pre-injury level of function. A patient who is not very active might tolerate a foot that is not normal. On the other hand, a patient whose job or recreational activities require a lot of walking or climbing may require major lifestyle and career changes.
Common Problems
Common problems that may persist after recovery include:
- Skin irritation. Footwear can irritate the skin or tendons in the affected area.
- Altered gait. In some cases, the arch of the foot has not been restored, or the Achilles tendon has not healed at its normal distance from the ankle. Full motion between the talus and the calcaneus is rarely regained in these cases, and this can change the way you walk. You may have problems walking on uneven ground, such as grassy surfaces or hills.
- Pain. After a fracture, you may experience continued subtalar pain and limited motion. Even if the heel anatomy is perfectly restored, you may still have discomfort. This can happen because of injured soft tissues, persistent fracture displacement, arthritis, or limited ankle and subtalar range of motion. Although relatively uncommon, pain can also be caused by irritation from the plates or screws.
Further Treatment
If you have chronic pain or experience other complications, you may need further treatment. This may include:
- Orthotics. A simple shoe modification may help some chronic problems. You may need to wear a heel pad, lift, or shoe cup, as well as special shoes with extra depth in the toe compartment.
- Additional surgery. Sometimes, another major operation is required. If the bone has healed in a deformed position, or if the subtalar joint becomes arthritic, the joint between the talus and the calcaneus may need to be fused. The goal of this procedure is to help the talus and the calcaneus grow together to form one bone. While this is very successful in reducing or eliminating pain, it results in limited hindfoot motion.
If the bone is badly deformed, your doctor may attempt to correct some or all of the deformity along with the fusion.
Improving Outcomes
There is no universal agreement among experts as to the best treatment method for calcaneus fractures. No single method works the same for everyone. Patients whose X-rays show good healing and normal heel anatomy often have ongoing symptoms after treatment. On the other hand, the calcaneus can look quite deformed on an X-ray, but the patient may have few, if any, symptoms.
Studies have compared results in patients whose fractures were treated with and without surgery. Some studies show a significant benefit of surgery, while other studies show less benefit for certain patients. Researchers continue to look for ways to improve the outcomes of treatment for different types of calcaneus fractures, as well as for patients who smoke or have other health considerations.
Your doctor will talk with you about the best treatment options in your case.
Contributed and/or Updated by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.