Diseases & Conditions
Brachial Plexus Injuries
The brachial plexus is a network of intertwined nerves that control movement and sensation in the arm and hand. A traumatic brachial plexus injury involves sudden damage to these nerves, and may cause weakness, loss of feeling, or loss of movement in the shoulder, arm, or hand.
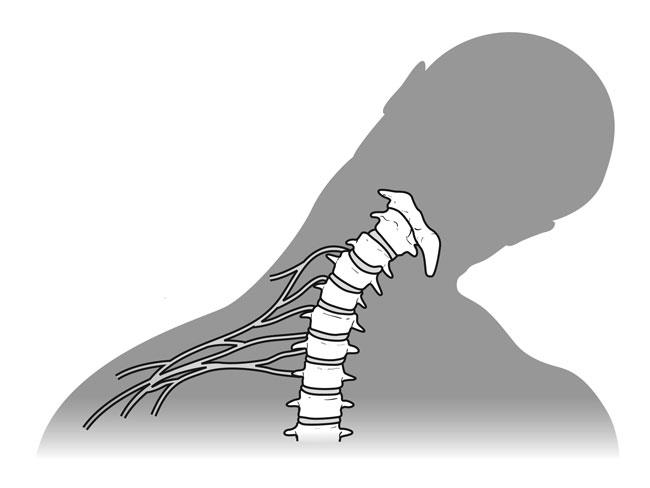
The brachial plexus begins at the neck and crosses the upper chest to the armpit. Injury to this network of nerves often occurs when the arm is forcibly pulled or stretched.
Mild brachial plexus injuries may heal without treatment. More severe injuries may require surgery to regain function of the arm or hand.
Anatomy
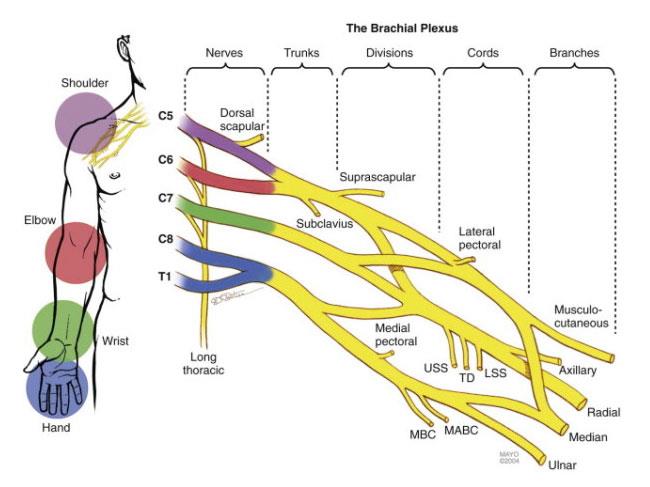
The brachial plexus is formed from five nerves that originate in the spinal cord at the neck. The plexus connects these five nerves with the nerves that provide sensation (feeling) to the skin and permit movement in the muscles of the arm and hand. There is a brachial plexus on each side of the body.
Each of the five nerves in the brachial plexus has a specific function, such as powering muscles or carrying sensory information from the hand to the brain. Because each nerve has a function, the location of the nerve injury within the plexus is important for predicting outcomes and for planning treatment.
The brachial plexus has 5 anatomic sections, and injuries to the brachial plexus can occur in one or more of these areas:
- Spinal nerves
- Trunks
- Divisions
- Cords
- Branches
Cause
Most traumatic brachial plexus injuries occur when the arm is forcefully pulled or stretched. Many events can cause the injury, including falls, motor vehicle collisions, knife and gunshot wounds, and most commonly, motorcycle collisions.
It is not known exactly how many brachial plexus injuries occur each year, but the number seems to be growing worldwide. Increased participation in high-energy sports and higher rates of survival from high-speed motor vehicle collisions may be factors in the growing number of these injuries.
Description
Brachial plexus injuries vary greatly in severity, depending upon the type of injury and the amount of force placed on the plexus. The same patient can injure several different nerves of the brachial plexus in varying severity.
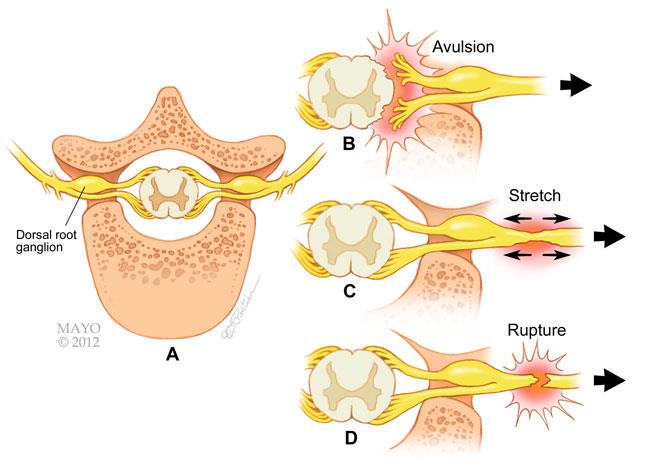
- Avulsion. This is the most severe brachial plexus injury. The nerve root has been pulled out of the spinal cord; this medically referred to as an "avulsion" injury. These types of injuries may not be repairable with standard surgeries.
- Stretch (Neuropraxia). When the nerve is mildly stretched, it may heal on its own or require simple, nonsurgical treatment methods to return to normal function.
- Rupture. A more forceful stretch of the nerve may cause it to tear partially or fully. These types of injuries can sometimes be repaired with surgery.
Upper-Trunk Palsy Injury
Upper-trunk palsy occurs when the angle between the shoulder and the neck forcibly widens, such as when a fall forces the shoulder down and the head to the opposite side.
Patients with upper-trunk palsies are unable to use the shoulder to raise the arm away from the body, have weakness in the arm, and may be unable to bend the arm at the elbow. There may be loss of sensation in the shoulder, outside of the arm, and thumb.
A severe upper-trunk injury may paralyze the shoulder muscles (deltoid muscle and rotator cuff), as well as the muscle in the upper arm (biceps.)
Lower-Trunk Palsy Injury
Lower-trunk palsy occurs when the angle between the arm and the chest wall forcibly widens. This may damage the lower nerves and the lower trunks.
Patients with a lower-trunk palsy will typically maintain shoulder and elbow strength, but will lose hand function. Over time, this will cause the fingers to contract into a claw position, and the patient will not be able to perform fine motor tasks. Patients also typically have hand numbness in at least the ring finger and small finger.
Pan-Plexus Palsy Injury
Pan-plexus palsy may occur if the force of the injury is extreme. In pan-plexus palsy, all levels of the nerves and trunk are damaged. This results in complete paralysis of the arm and hand, which is often referred to as "flail limb."
Gunshot Wounds
Brachial plexus injuries caused by a gunshot wound do not typically damage the nerve severely.
The severity of injury will depend on the bullet's caliber, velocity, and angle of entry.
- Low-velocity bullets typically damage nerves by impacting them directly.
- High-velocity bullets can injure nerves by direct impact (bruising) or, more commonly, by shockwaves that stretch the nerve. A nerve stretching and bruising injury will often recover on its own.
Gunshot wounds may also cause artery or vein injuries that require immediate or delayed repair.
Penetrating Wounds
A brachial plexus injury caused by a penetrating wound, such as a knife wound (laceration), may damage or cut the nerve. This type of injury to the nerve will not typically recover on its own, prompting more immediate treatment.
Additional Injuries
Because brachial plexus injuries are typically caused by high-energy, forceful events, many patients have additional injuries. These may include artery or vein injuries, fractures to the shoulder or arm, rib fractures, a collapsed lung, bleeding into the lungs or chest cavity, spine fractures, spinal cord injury, and traumatic brain injury.
Symptoms
Symptoms vary depending upon the type and location of the injury to the brachial plexus as well as whether the patient sustained other injuries. The most common symptoms of brachial plexus injury include:
- Weakness or numbness
- Loss of sensation
- Loss of movement (paralysis)
- Pain
The pain from brachial plexus injuries results from injury to the spinal cord where the nerve rootlets are pulled out of the cord. This pain is neuropathic in nature; it can be very difficult to deal with and can last for a very long time.
Brachial plexus injuries that occur at the level of the spinal cord often produce greater pain than injuries farther from the spinal cord. In addition, injuries nearer the spinal cord may cause a burning numbness, which is called paresthesia or dysesthesia.
Doctor Examination
Patients with brachial plexus injuries must be evaluated and treated within an appropriate timeframe, typically within 6 to 7 months after injury. The longer a muscle is without nerve input, the less likely it is that the muscle will function normally in the future. This is true even if the muscle eventually recovers its nerve signals.
The exact timeframe for seeking treatment depends on the type of injury and its location.
Physical Examination
If your doctor suspects a brachial plexus injury, they will perform a comprehensive examination to diagnose the injury and determine whether any associated injuries exist. They will examine all nerve groups controlled by the brachial plexus to identify the specific location of the nerve injury and its severity.
The pattern by which nerves from the brachial plexus control various muscles of the arm and hand will assist your doctor in identifying potential sites of nerve injury. Your doctor will examine all nerve groups controlled by the brachial plexus.
In addition, some patients display specific signs that help determine the location of the nerve injury:
- Narrowing of the eye pupils, drooping of the eyelid, and lack of ability for the face to sweat (Horner's syndrome) are signs that the injury is close to the spinal cord.
- A shooting nerve-like pain when the doctor taps along the affected nerves (Tinel's sign) suggests an injury farther from the spinal cord. If the location of the Tinel's sign moves down the arm toward the hand over time, it is a sign that the injury is repairing itself.
During the physical examination, your doctor will also assess your arm and shoulder for stability and range of motion.
Imaging Tests
X-rays. X-rays create clear pictures of dense structures, like bone. X-rays of the neck, chest, shoulder, and arm are taken to rule out associated fractures. Chest X-rays are obtained to look for rib fractures or lung injury. If you are not able to take a full, deep breath during the chest X-ray, your doctor may consider pulmonary function testing with the assistance of a pulmonologist to rule out damage to the nerves that control deep breathing.
Computed tomographic (CT) scan. A CT scan is considered the most reliable test for detecting spinal nerve avulsion (pull out) injuries. Contrast dye is injected around the spinal cord in the neck to more clearly show the injury on the CT image. CT is typically performed at least 3 to 4 weeks after the injury to allow any potential blood clots around the nerve root to dissolve. Some centers may also use magnetic resonance imaging (MRI) scan instead of, or in addition to, a CT scan.
Electrodiagnostic studies. These tests measure nerve conduction and muscle signals. They are important evaluation tools because they can confirm the diagnosis, locate the nerve injury, characterize its severity, and assess the rate of nerve recovery. A baseline electrodiagnostic examination is done 3 to 4 weeks after the injury. This allows any nerve degeneration that may occur to become detectable. Electrodiagnostic studies are repeated 2 to 3 months after the initial study and then repeatedly over time to assess whether the nerves are recovering.
Nonsurgical Treatment
Many injuries to the brachial plexus will recover spontaneously without surgery over a period of weeks to months, especially if they are mild. Nerve injuries that heal on their own tend to have better functional outcomes. If your doctor believes that the injury has a good potential for recovery without surgery, they may delay procedures and simply monitor your injury.
The process of the nerve healing itself takes time, and your doctor may recommend physical therapy to prevent joint and muscle stiffness.
Surgical Treatment
Surgical treatment is typically recommended when the nerves fail to recover on their own or fail to recover enough to restore necessary function to the arm and hand. It is important to note that depending on the severity of the injury, even surgery may not be able to return the arm or hand to normal.
Considerations
Recovery. During your discussion with your doctor, it will be important to set realistic goals and expectations for surgical treatment. Nerves heal slowly. The recovery period after surgery is often long and requires a strong commitment to a comprehensive rehabilitation program to restore physical abilities. This is something you should consider when making the decision about whether to proceed with surgery.
Candidates for surgery. Although brachial plexus surgery can help to restore function in many patients, there are some factors that prevent a patient from being a candidate for surgery, most importantly, unrealistic expectations. Other factors include:
- Having joint stiffness and contractures
- Advanced age
- Additional injuries or medical conditions
- Having a traumatic brain injury or spinal cord injury
Your doctor will discuss with you whether you are a candidate for surgery.
Complications.
- It is possible that surgical treatment will not restore desired movement or that the surgical wound may become infected. Both of these outcomes could require further surgery.
- Patients with pre-existing medical problems have additional potential risks related to any large reconstructive surgery, including chronic pain, blood clots, heart attack, stroke, and even death.
Surgical Procedures
Several surgical techniques are used to treat nerve injury, depending on the type of injury and the length of time that has passed since the injury.
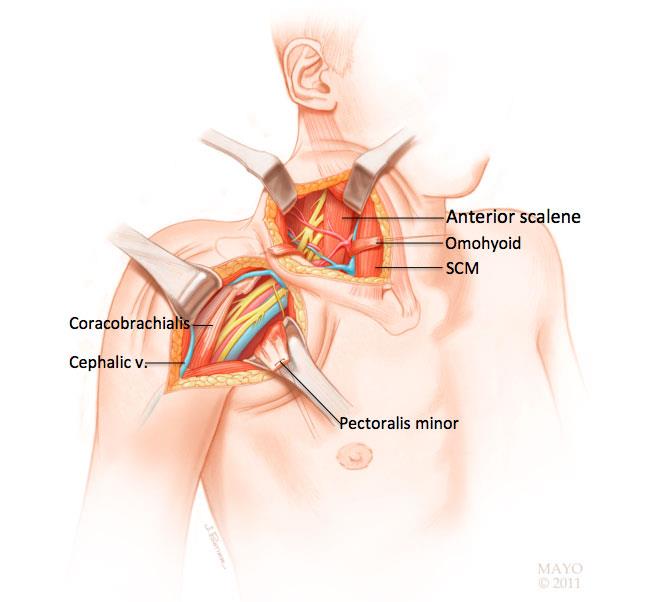
In most procedures, the surgeon makes an incision near the neck above the collarbone. If the injury extends down the brachial plexus, the surgeon may need to make another incision at the front of the shoulder. To repair or reconnect nerves, surgeons often use high-powered microscopes and small, specialized instruments.
Nerve repair. In this procedure, the surgeon reattaches the two torn edges of a severed nerve. Nerve repair is typically performed immediately for sharp lacerations to the nerves, such as from a knife wound.
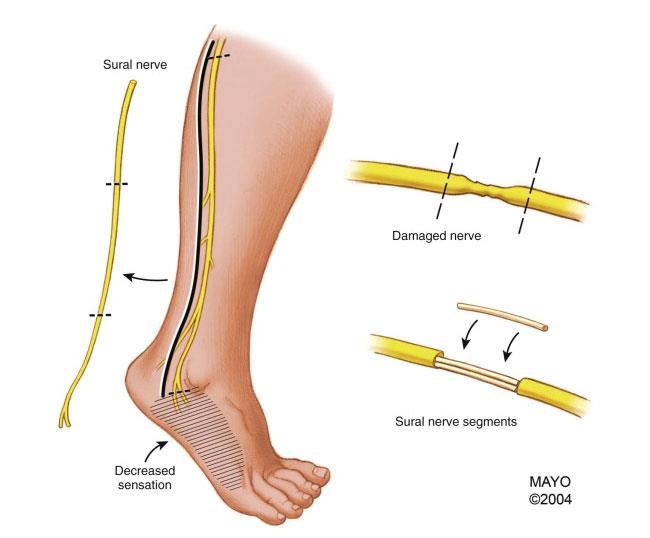
Nerve graft. Nerve grafting is a procedure in which a healthy nerve taken from another part of the body is sewn in between the two ends of a ruptured nerve. The transplanted nerve acts as a scaffold to support the injured ends as they regenerate and grow back together. Nerve grafting can be performed only if there is a functioning nerve stump at the spinal cord to conduct a nerve signal. The goal is for the transplanted nerve to guide nerve regrowth and ultimately restore nerve signals to power the paralyzed muscles.
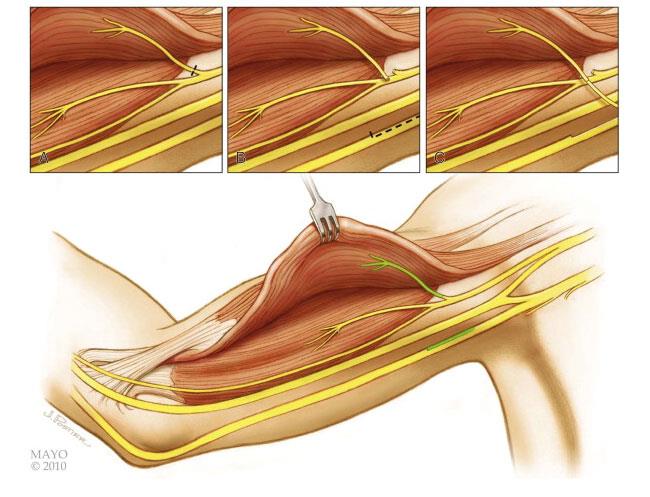
Nerve transfer. A nerve transfer procedure is used when there are no functioning nerve stumps in the neck to which nerve grafts can be connected. In this procedure, a healthy donor nerve is cut and reconnected to the injured nerve to provide a signal to a paralyzed muscle. In many cases, the healthy nerve is connected closer to the affected muscle. In other cases, the healthy nerve is connected to the damaged nerve within the brachial plexus.
Tendon and muscle transfers. Patients who delay that first visit to the doctor for more than 12 months after injury tend to have poor outcomes with surgery to reconstruct or repair nerves. These patients are managed better with surgery that focuses on reconstructing the tendon (tendon transfer) or muscle (free-functioning muscle transfer).
A tendon transfer is procedure in which the tendon of a functioning muscle is cut and sewn into a nonfunctioning muscle tendon to restore a specific motion or motor function.
In a free-functioning muscle transfer, a muscle from one part of the body is moved to the injured area, along with its tendon, artery, vein, and nerve. Each of these structures is connected to the corresponding structures of the injured area to restore motion or motor function.
Recovery and Rehabilitation
Because nerve regeneration occurs slowly at a rate of approximately 1 mm/day, recovery from a brachial plexus injury takes time, and patients may not experience results for several months. A positive mindset and the support of family, friends, and healthcare professionals are important to recovery and rehabilitation.
During this recovery process, occupational therapists teach patients how to use the unaffected arm to perform daily activities like eating and personal hygiene.
Physical therapy of the shoulder, elbow, wrist, and fingers involves specific exercises to prevent stiffness, contractures, or muscle atrophy. A physical therapist can also recommend assistive devices, such as splinting or supportive bracing to help support a limp arm and joints. Compression gloves and sleeves may be used to prevent swelling in the affected arm, which can lead to pain and joint contractures.
Pain may be managed with medications, therapy, and/or assistive devices.
In addition, patients will require healthy coping skills to adjust their lives — both in terms of employment and daily activities — in anticipation of a less functional arm and/or hand.
Future Developments
Although brachial plexus injuries can be devastating and difficult to manage, a team approach to treatment has made significant improvements in patient function. Although current technology cannot return patients with a flail limb to their preinjury state, restoring some function to the arm is a major advance.
Future developments in treatment of these injuries include newer techniques for repairing or transferring nerves, as well as new medications or materials to help promote and stimulate healthy nerve regeneration.
Last Reviewed
March 2022
Contributed and/or Updated by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.