Diseases & Conditions
Biceps Tendinitis
This article was written and/or reviewed by a member of American Shoulder and Elbow Surgeons (ASES).
Biceps tendinitis is an inflammation or irritation of the upper portion of the biceps tendon, also called the long head of the biceps tendon. The biceps tendon is a strong, cord-like structure that connects the biceps muscle to the shoulder socket.
Common symptoms of biceps tendinitis include pain in the front of the shoulder and weakness with movement of the shoulder. This can often be relieved with rest and medication. In severe cases, you may need surgery.
Anatomy
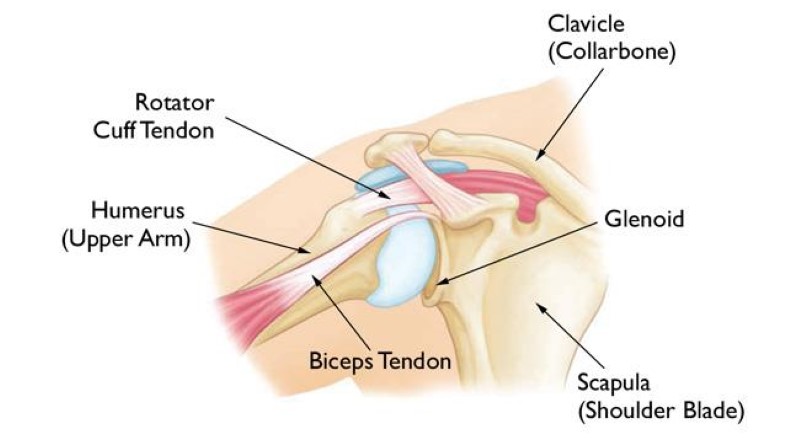
The shoulder is a ball-and-socket joint made up of three bones:
- The humerus (upper arm bone)
- The scapula (shoulder blade)
- The clavicle (collarbone)
Glenoid. The head of the humerus fits into the rounded socket in the scapula. This socket is called the glenoid. The glenoid is lined with soft cartilage.
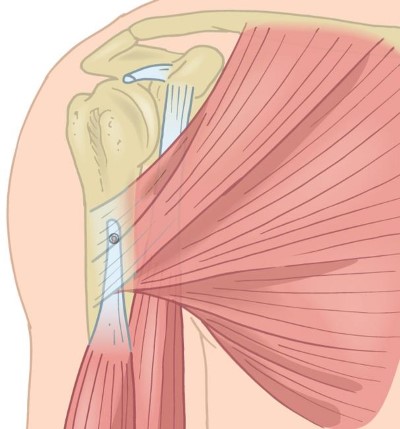
Rotator cuff. A combination of muscles and tendons keep the arm centered in the shoulder socket. These tissues, called the rotator cuff, cover the head of the upper arm bone and attach it to the shoulder blade.
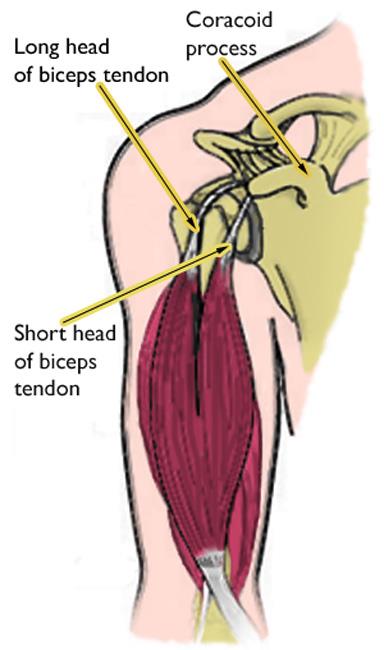
Biceps tendons. The biceps muscle is in the front of the upper arm. It has two tendons that attach it to the shoulder blade bone.
- The long head attaches to the top of the glenoid (shoulder socket).
- The short head attaches to a bump on the front of the shoulder blade called the coracoid process.
Description
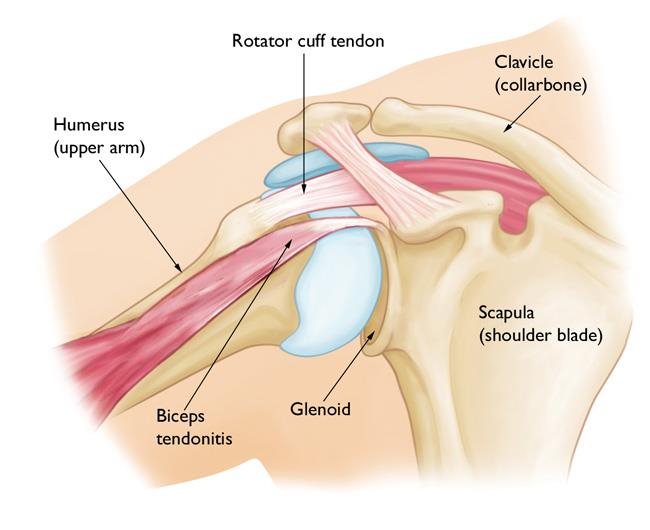
Biceps tendinitis is inflammation of the long head of the biceps tendon.
- In its early stages, the tendon becomes inflamed and swollen.
- As inflammation progresses, the tendon and its sheath (covering) can become more irritated, which causes it to thicken.
- Occasionally, in the late stages, the damage to the tendon can result in fraying or a complete tear. A complete tendon tear results in a cosmetic deformity of the arm (a "Popeye" bulge in the upper arm).
Biceps tendinitis usually occurs along with other shoulder problems, such as:
- Rotator cuff degeneration and/or tearing
- Arthritis of the shoulder joint
- Tears in the glenoid labrum (the soft fibrous ring of tissue that surrounds the glenoid and helps to stabilize the shoulder joint)
- Chronic shoulder instability (multiple dislocations)
- Other diseases that cause inflammation of the shoulder joint lining
Cause
In most cases, damage to the biceps tendon is due to a lifetime of normal activities. As we age, everyday wear and tear causes our tendons to slowly weaken. This degeneration can be worsened by overuse — repeating the same shoulder motions again and again.
Many jobs and routine chores can cause overuse damage. Sports — especially those that require repetitive overhead motion, such as swimming, volleyball, pickleball, tennis, and baseball — can also put people at risk for biceps tendinitis.
Symptoms
- Pain or tenderness in the front of the shoulder, which worsens with overhead lifting or activity
- Pain with reaching backward, such as to put on your seatbelt in a car or to put a coat on
- Pain or achiness that moves down the upper arm bone
- An occasional snapping sound or sensation in the shoulder
Doctor Examination
Physical Examination
After discussing your symptoms and medical history, your doctor will examine your shoulder.
During the examination, your doctor will:
- Assess your shoulder for range of motion, strength, and signs of shoulder instability
- Possibly palpate (push on) the front of your shoulder directly over your biceps tendon
- Perform specific physical examination tests to check the function of your biceps
Imaging Tests
Tests that may help your doctor confirm your diagnosis include:
X-rays. Although they only visualize bones, X-rays may show other problems in your shoulder joint.
Magnetic resonance imaging (MRI) and ultrasound. These imaging techniques can show soft tissues like the biceps tendon in greater detail than X-rays. In particular, these tests may help show:
- How irritated the tendon is
- How much inflammation is present
- Whether the tendon is torn
Treatment
Your orthopedic surgeon will work carefully to identify any other problems in your shoulder and treat them along with your tendinitis.
Nonsurgical Treatment
Biceps tendinitis is typically first treated with nonsurgical methods. This type of nonsurgical treatment is very effective in most patients.
Rest. The first step toward recovery is to avoid activities that cause pain.
Ice. Apply cold packs for 20 minutes at a time, several times a day, to keep swelling down. Do not apply ice directly to the skin.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs like ibuprofen, aspirin, and naproxen can reduce pain and swelling.
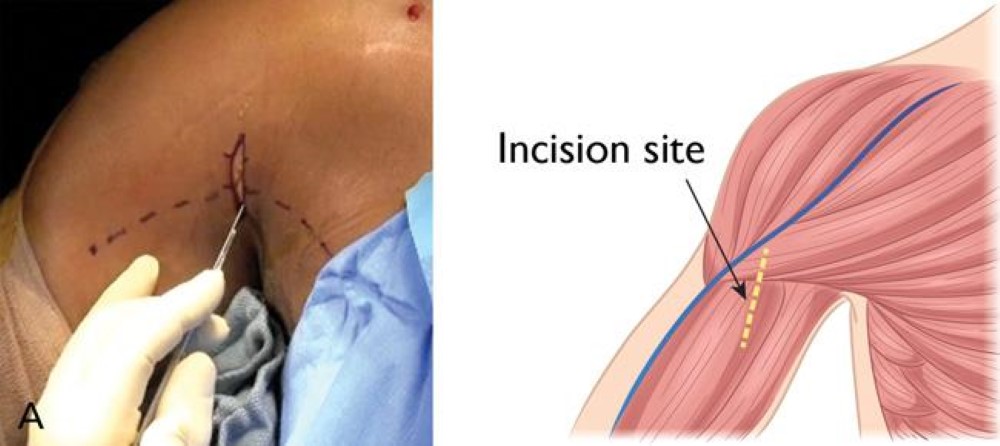
Steroid injections. Steroids such as cortisone are very effective anti-inflammatory medicines. Injecting steroids into the tendon can relieve pain. Your doctor will discuss whether you are a candidate for an injection. Given the location of the tendon within its sheath, these injections are often done under image guidance, such as with an ultrasound. Learn more: Cortisone Shot (Steroid Injection)
Physical therapy. Specific stretching and strengthening exercises can help restore range of motion and strengthen your shoulder.
Surgical Treatment
If your condition does not improve with nonsurgical treatment, or improved but then comes back, your doctor may offer surgery as an option. Surgery may also be an option if you have other associated shoulder problems.
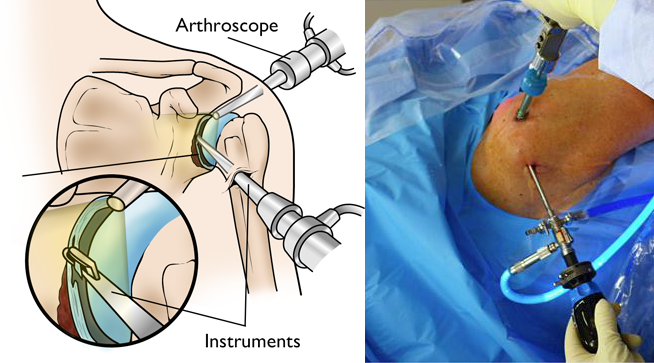
Surgery for biceps tendinitis is usually performed arthroscopically. This allows your doctor to assess the condition of the biceps tendon as well as other structures in the shoulder.
During arthroscopy, your surgeon inserts a small camera, called an arthroscope, into your shoulder joint. The camera displays pictures on a monitor, and your surgeon uses these images to guide miniature surgical instruments.
Repair. Rarely, the biceps tendon can be repaired where it attaches to the shoulder socket (glenoid). This is the least common treatment method and is usually reserved for young, very active, high-demand patients.
Biceps tenodesis. In some cases, the damaged section of the biceps is removed, and the surgeon reattaches the remaining tendon to the humerus (upper arm bone). This procedure is called a biceps tenodesis. Removing the painful part of the biceps usually resolves symptoms and restores normal function.
Depending on your situation, your surgeon may choose to do this procedure arthroscopically or through a small open incision in the front of your shoulder.
Tenotomy. In some cases, the long head of the biceps tendon may be so damaged that it is not possible to repair or tenodese it. Your surgeon may simply elect to release the damaged biceps tendon from its attachment to bone. This is called a biceps tenotomy.
This option is the least invasive but may result in a Popeye bulge in the arm.
Patients who have tenotomy usually do well and return to near normal strength. This surgery also has the shortest recovery time.
Surgical complications. Overall, complication rates are low.
Possible complications and post-surgery issues include:
- Infection
- Stiffness
- If a tenodesis was performed, possible rupture of the tendon and/or pain where the tendon was reattached
- If a tenotomy was performed, possible cramping in the muscle
Rehabilitation. After surgery, your doctor will prescribe a rehabilitation plan based on the procedures performed. You may wear a sling for a few weeks.
Your doctor may restrict certain activities to allow the repaired tendon to heal. It is important to follow your doctor's directions after surgery to avoid damage to your repaired biceps.
Your doctor will start you on therapeutic exercises a few weeks after surgery. They may refer you for physical therapy, but PT is not always necessary.
- Flexibility exercises will improve range of motion in your shoulder.
- Exercises to strengthen your shoulder will gradually be added to your rehabilitation plan.
Surgical outcome. Most patients have good results. They typically regain full range of motion and are able to move their arms without pain.
People who play very high-demand overhead sports occasionally need to limit these activities after surgery.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.