Diseases & Conditions
Achilles Tendon Rupture (Tear)
Tendons are cords of fibrous tissue that form strong attachments between muscles and bones. The Achilles tendon works with the muscles of your calf to help provide strength during walking, running, and other activities. It helps push the foot and ankle down into the ground, an action referred to as "plantarflexion." This movement helps lift your heel off the ground and stand on the tips of your toes.
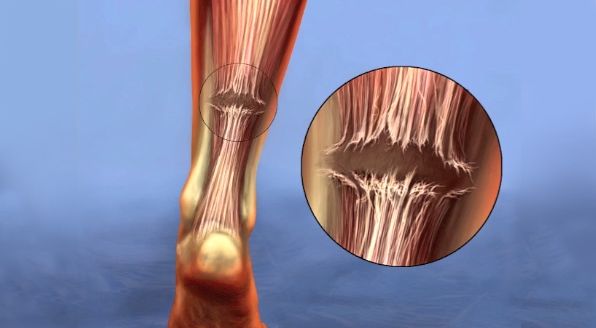
Small tears in the Achilles tendon can be bothersome and can cause pain during activity. However, a large or full tear of the Achilles tendon is a disabling injury.
Achilles tendon tears often occur from an injury to the tendon. The tears can be treated without surgery at times; however, a surgeon may recommend surgery to repair the tendon.
Anatomy
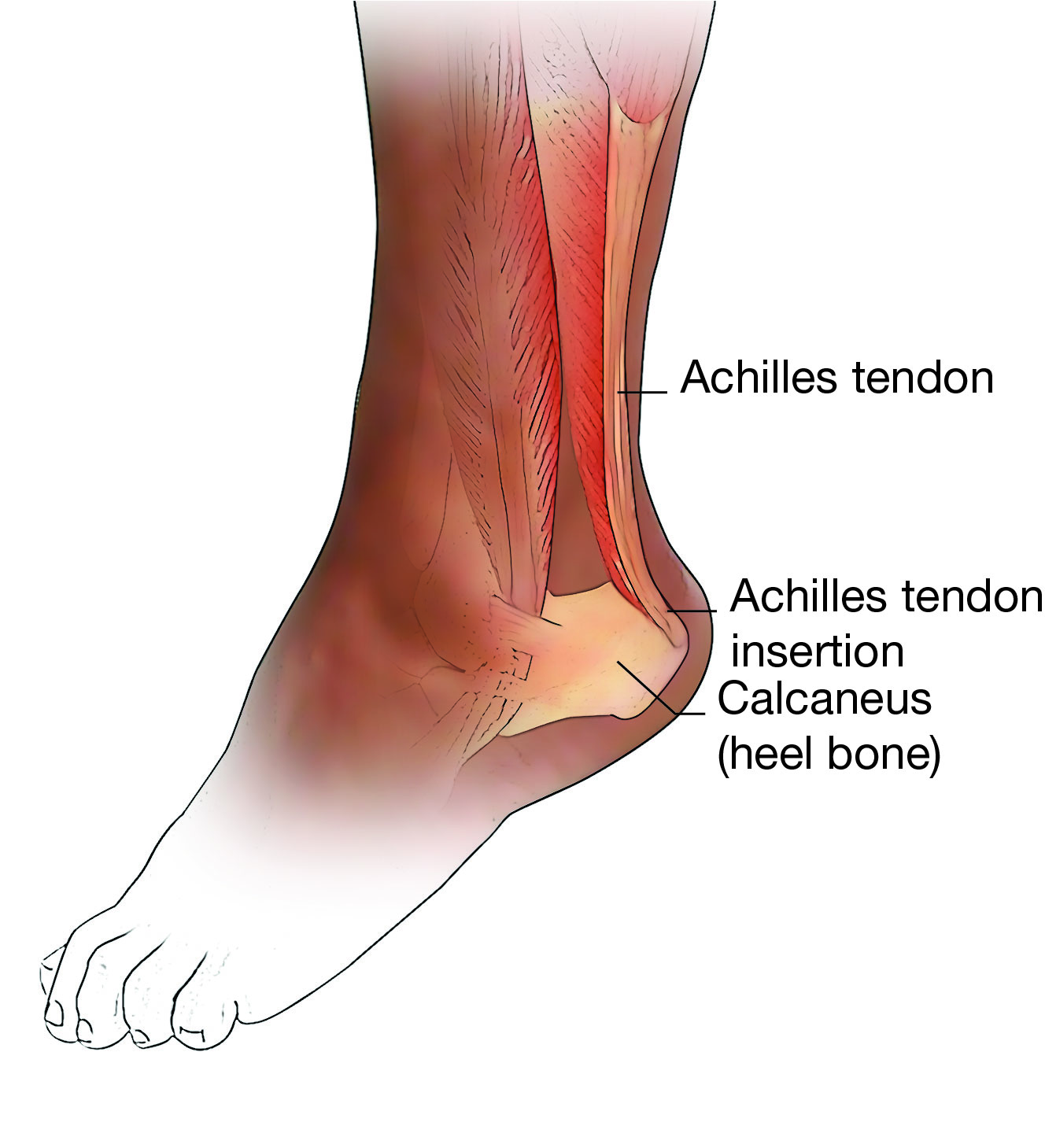
The Achilles tendon can be thought of as a continuation of the calf muscles. It attaches at the back of the calcaneus (heel bone). Because of the strength and repetitive use of the calf muscles, the Achilles tendon is the largest tendon in the body.
The central (middle) part of the Achilles tendon is thought to have a poor blood supply compared to the other parts of the tendon. This part of the tendon is found roughly 2 ½ inches from where the tendon attaches to the heel bone.
Description
Achilles tendon tears can be either partial or complete.
- Partial tears. If a tear does not completely disrupt the tendon, it is called a "partial tear." You can think of this like a stretched rope, where some of the fibers are frayed, but the rope is still in one piece. Partial tears of the Achilles tendon are rare compared to complete tears.
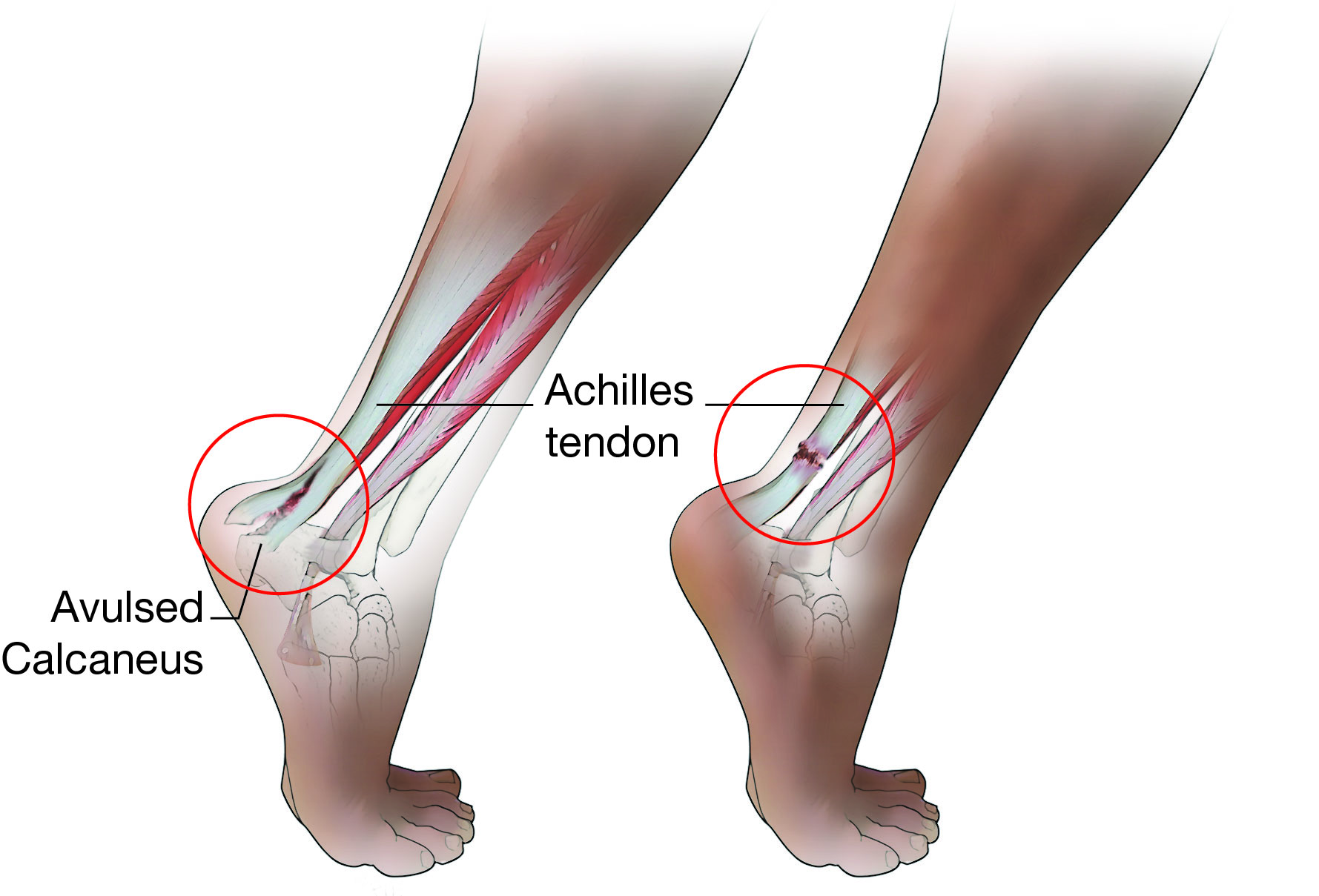
- Complete tears. The Achilles tendon can be completely torn when exposed to high enough stress. It will either tear from its insertion (attachment site) on the heel bone, or tear at some point in the middle of the tendon. Without this tendon in one piece, you may not be able to lift your body up onto your toes on the injured leg.
Cause
Injury
A very strong force is needed to tear the Achilles tendon. Typically, Achilles tendon tears occur when the calf muscle is stretched too quickly.
- This can occur when landing from a jump or during cutting movements in a sport.
- In sports like football or soccer, Achilles tendon tears can also happen when an athlete steps on the heel bone of another athlete.
Tendon Weakness
A weakened Achilles tendon is more likely to tear. Several things can lead to tendon weakness.
Corticosteroid injections to treat Achilles tendinitis have been linked to an increased risk of tendon rupture. Because of this, doctors avoid giving these injections in or around the Achilles tendon.
Chronic disease. Many diseases can disrupt blood supply and cause inflammation throughout the body. These diseases, which include the following, can weaken tendons:
- Inflammatory diseases (rheumatoid arthritis, systemic lupus erythematosus)
- Diabetes mellitus
- Infection
- Obesity
- Metabolic disease
Medication use. Use of certain antibiotics such as ciprofloxacin (Cipro) or levofloxacin (Levaquin) has been linked with tendon tearing. Also, medications like corticosteroids and anabolic steroids have been linked to increased muscle and tendon weakness.
Symptoms
- When an Achilles tendon tears, you may hear a popping noise.
- Severe pain and swelling near the heel can follow, and you may not be able to walk on that injured leg.
- You may find you are unable to stand up on the toes of the injured leg.
Doctor Examination
Medical History and Physical Examination
Your doctor will ask about the symptoms around your heel that you are experiencing. They will also discuss your general health and your medical history. They may ask questions like these:
- Do you have any medical conditions that might put you at risk for a tendon injury?
- Do you have Achilles tendinitis, or have you had previous pain in this Achilles tendon?
- Do you take any medications that may increase the risk of a tendon injury?
- Have you had previous surgery on this foot, ankle, or Achilles tendon?
After discussing your symptoms and medical history, your doctor will conduct a thorough examination of your Achilles tendon:
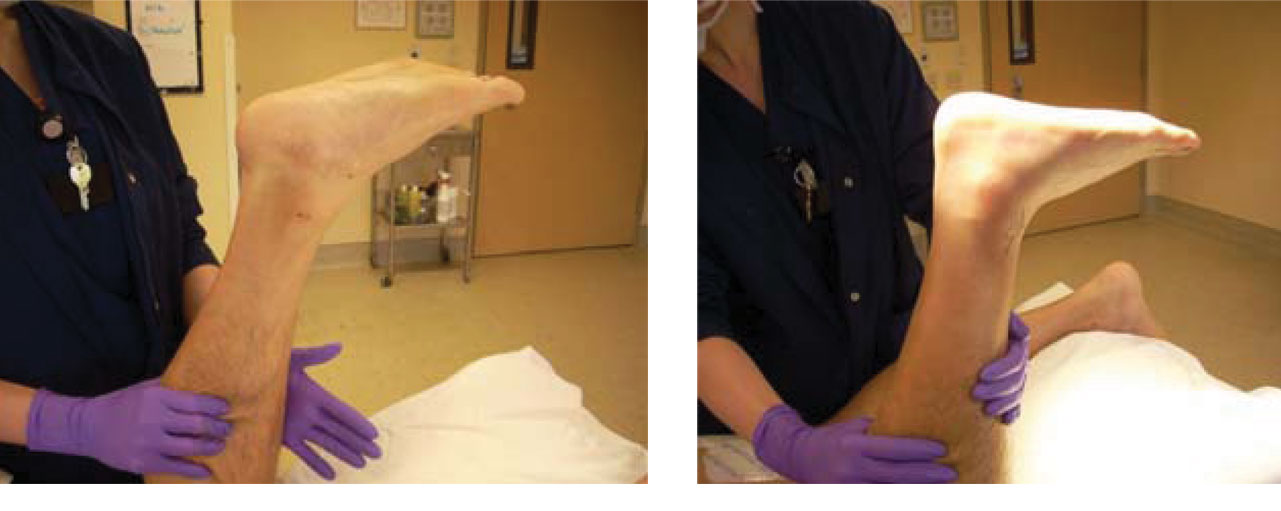
- They may ask you to attempt to stand on your toes.
- They may ask you to bend your ankle or push down on their hand.
- They may perform a test where they squeeze your calf and see how the foot responds to this squeeze. This is called the Thompson test.
Parts of this examination may cause pain, but the tests are needed to correctly identify a tear.
Imaging Tests
Your doctor may order some imaging tests, such as an X-ray, ultrasound, or magnetic resonance imaging (MRI) scan.
X-rays. If the Achilles tendon tears from the insertion (attachment site) on the heel bone, the doctor may see a fleck of bone on the X-ray. This can be very helpful in making the diagnosis.
Ultrasound. An ultrasound can show the tendon in real time and will be able to determine both if there is a tear and, if so, how it responds when the ankle is moved. This can help your doctor understand the nature and size of the tear.
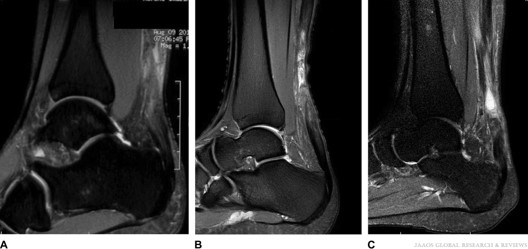
Magnetic resonance imaging (MRI) scan. While an X-ray gives doctors a clear view of bones, an MRI provides a better image of the soft tissues, such as tendons. The MRI can:
- Show the amount of tendon torn and the location of the tear.
- Help your doctor rule out a different injury that may have similar symptoms.
- Reveal if there was inflammation in the tendon prior to the tear.
Treatment
Your doctor will consider several things when planning your treatment, including:
- Whether your tear is partial or complete
- Your activity level
- Your age
- Your occupation
There is currently a debate among surgeons about whether or not to treat Achilles tendon tears with surgery.
- Small, partial tears respond well to nonsurgical treatment.
- Complete tears can be treated nonsurgically. However, there are many factors that may influence a surgeon to recommend an operation to repair the tendon.
The decision to perform surgery or not for an Achilles tendon tear is complex and personal.
Nonsurgical Treatment
Immobilization. Your doctor will recommend that you wear a brace/boot, splint, or cast in a position where your toes are pointed toward the ground. This will keep your Achilles tendon in a stable position to help it heal. You will need crutches or a wheelchair to get around. You will not be able to walk on the injured leg.
Different doctors will recommend different amounts of time for healing. However, you should plan to be immobilized in a boot for at least 6 weeks.
Physical therapy. After the Achilles tendon has begun to heal, you will begin physical therapy. Therapists are well trained in slowly increasing your activity and the motion through the ankle to avoid injury to the newly healed tendon.
Surgical Treatment
Surgical treatment of Achilles tendon tears is the topic of much ongoing research. A surgeon may recommend surgical repair of the tendon if:
- You are a competitive athlete
- Jumping and pushing off with your toes are critical to your activities. Some of this pushing off strength can impact running and jumping.
Some studies have shown improved pushing off strength in patients who have surgical treatment for their Achilles tendon tear. Other studies suggest that patients who have surgical repair are less likely to re-tear their Achilles than patients who allow the tendon to heal without surgery. There is still debate about these findings, and research is ongoing.
People who do end up having surgery will have better outcomes if the repair is performed soon after the injury. This is because the tendon will begin to shorten and scar over time, which can make the procedure more difficult.
Procedure
The surgery may be performed with regional anesthetic, which numbs only your surgical leg, or general anesthetic, which puts you to sleep.
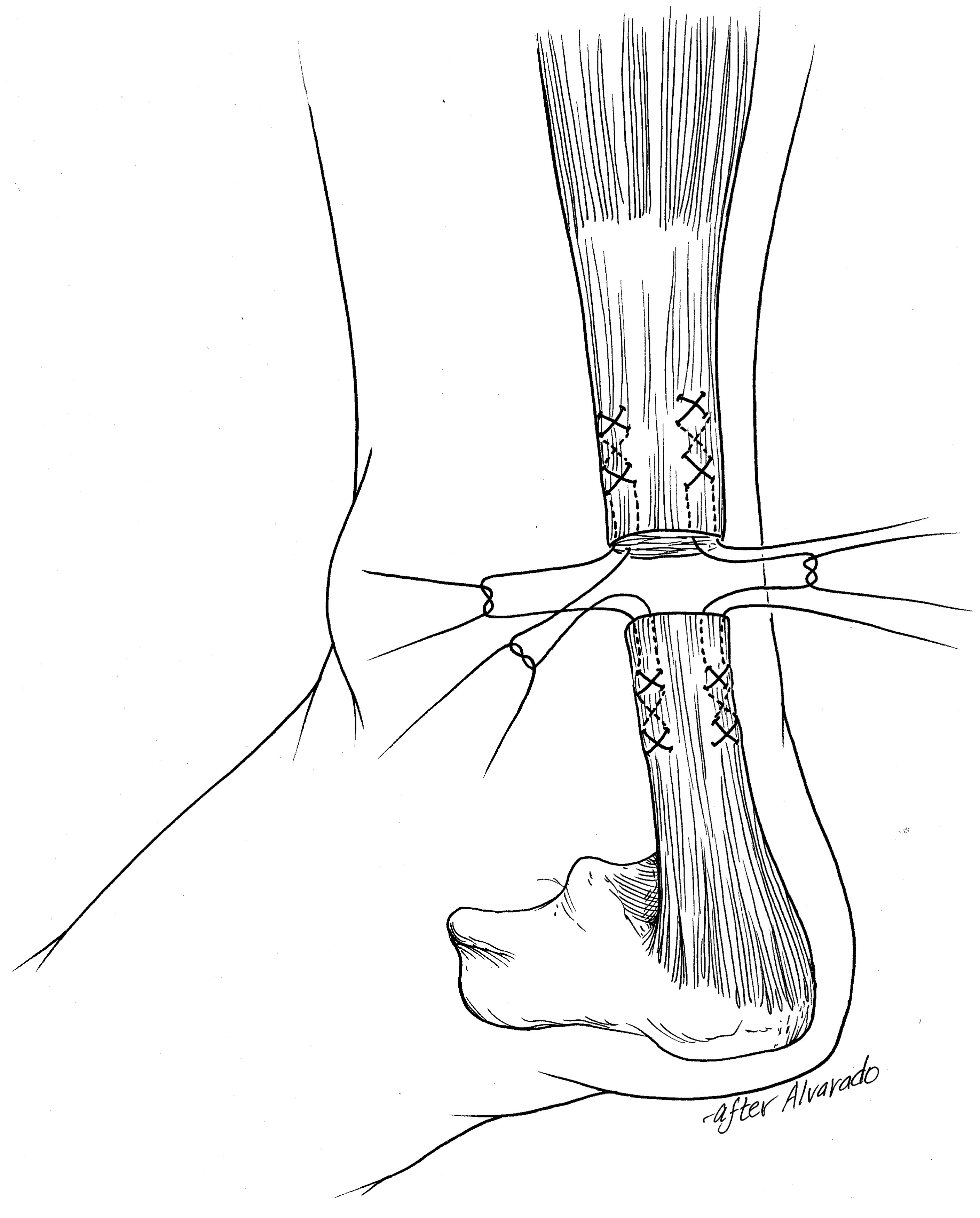
- If the Achilles tendon ruptured from the insertion (attachment site) on the heel, surgeons will tack the tendon back down to the heel using anchor devices, which are drilled into the heel bone.
- Tears of the middle part of the tendon are repaired using sutures to bring the torn edges together. There are several techniques which can be used to perform this repair. Your surgeon can discuss these options with you. Newer techniques involve smaller skin incisions, and these are referred to as "minimally invasive surgery (MIS)."
Considerations
Tendons can shorten and scar if too much time has passed since the injury. In this instance, surgeons sometimes have to add donated tissue (allograft) to the repair to bridge the gap. Often, this can be predicted, and the surgeon will discuss this with you before the surgery.
Complications
- As with any surgery, infection, nerve injury, wound breakdown, complications from the anesthesia, and blood clots can occur.
- Tearing of the Achilles tendon after repair is possible as well.
- Some patients may complain of continued pain and weakness when pushing off or jumping.
Recovery
- Your doctor will give you medication after the surgery to help with pain management.
- Your doctor may also recommend elevation of the injured leg.
- You will likely leave the hospital or surgery center on the same day of surgery and will be placed in a cast, brace/boot, or splint to immobilize the injured Achilles tendon.
- Several weeks after surgery, you will return to the surgeon's office to have the skin sutures removed.
- Most surgeons will again place either a cast, splint, or brace/boot after the sutures are removed.
- Different surgeons will suggest different amounts of time spent in the cast, splint, or brace/boot, but you can expect roughly 6 weeks of immobilization.
- Over time, your doctor or therapist will reduce use of your boot. This will allow you to begin range of motion. Gradually, strengthening exercises will be added to your rehabilitation plan to work on regaining pushing off strength.
- Complete recovery can take about 12 months. Some patients report that it takes closer to 2 years before they were able to reach all of their goals.
Outcomes
Most people can expect to return to their occupation (job) and activities of daily living after recovering from an Achilles tendon tear.
Regardless of the treatment, there is some loss of strength after an Achilles rupture; however, with focused strengthening and therapy, most patients are able to return to their previous level of activity. This can take up to 18 to 24 months after the injury.
Return to sport for athletes can involve a complex set of tests to ensure that the athlete is ready to participate in full activity.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.