Treatment
Prescription Drug Safety in Orthopaedic Surgery
Bone and joint injuries and surgeries can be painful. Orthopaedic surgeons are committed to helping their patients recover from injury and surgery and live as comfortably and with as little pain as possible, while also ensuring overall health and safety.
There are various ways to manage pain and discomfort after an orthopaedic injury or surgery. Patients and their doctors should work together to figure out the most effective and safest course of action. Depending on how serious the condition is, pain management strategies can include:
- Exercise and activities that boost physical and mental health
- Cold and hot compresses
- Over-the-counter pain medications, such as acetaminophen or non-steroidal anti-inflammatory drugs (NSAIDs)
- More powerful prescription opioids (also called narcotics)
When used as recommended, prescription painkillers can relieve severe pain, especially during the hours and days immediately after an injury or major surgery. However, opioids are not a long-term pain solution and, when misused, can lead to addiction and even death.
If an orthopaedic condition is causing prolonged (long-term) pain, your orthopaedic surgeon will refer you to other types of doctors, such as pain management specialists.
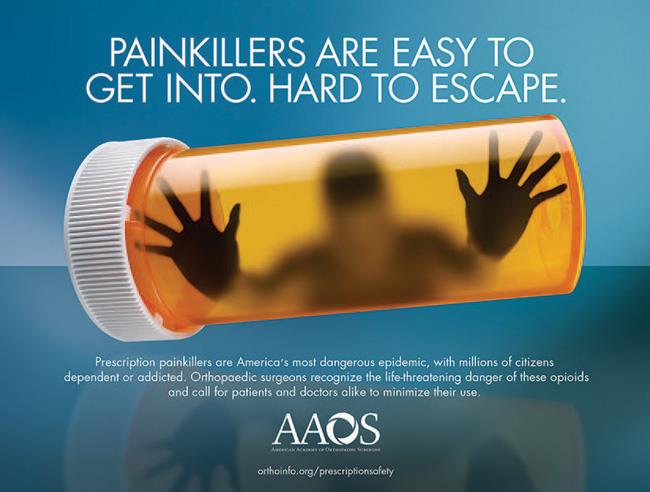
The Opioid Epidemic
Many studies and alarming data have exposed the side effects, addictive dangers, and devastating consequences of opioid use and misuse. In fact, the U.S. is still fighting an opioid epidemic, with millions of people dependent on or addicted to prescription painkillers such as codeine, morphine, oxymorphone, tramadol, hydrocodone, oxycodone, and oxycontin. A 2016 Washington Post/Kaiser Family Foundation survey found that 1 in 3 patients (34%) who recently took opioids for at least 2 months reported being addicted or dependent.
According to the U.S. Department of Health and Human Services:
- Since 1999, the rate of overdose deaths involving opioids — including prescription pain relievers and heroin — has nearly quadrupled.
- Since 1999, 760,000 people have died from a drug overdose. Two out of 3 overdose deaths (66%) in 2018 involved an opioid.
- In 2019 (the most recent year data is available), 9.7 million people misused prescription pain relievers, and more than 70,000 died from drug overdoses.
- On an average day in the U.S., more than 650,000 opioid prescriptions are dispensed, 3,900 people initiate nonmedical use of prescription opioids, and 78 people die from an opioid-related overdose.
In addition, patients already taking opioids before a surgical procedure have greater post-surgical pain, and face a higher risk of pneumonia, over-sedation, and even death.
How to Safely Manage Pain After Orthopaedic Surgery
Given the dangers of prescription opioids, how can orthopaedic patients safely and effectively manage pain?
The American Academy of Orthopaedic Surgeons and many high-volume orthopaedic care centers (those that treat a large number of patients) have led the way in fighting the opioid epidemic through research. This research has shown that a patient-centered and personalized multi-modal pain management program can minimize opioid use in everything from spine surgery to joint replacement to hand surgery. Here's what patients need to know and do:
- First, expect some tolerable discomfort (pain that you can bear). Pain is your body's early warning system and part of the normal healing process after surgery or an injury and will improve day-by-day. The first few days after a surgery or injury are typically the most intense, but pain will improve daily. Expecting a pain-free or numb experience can lead to overuse of medications.
- Pain from many injuries and surgeries will be well-managed with pain management alternatives to opioids.
- Splints, consistent use of ice or heat on and off the affected site, and non-opioid pain medications such NSAIDS (ibuprofen, naproxen, etc.) or acetaminophen are often enough to manage the pain and discomfort of many common injuries such as lacerations and fractures.
- Don't discount (dismiss) the powerful effects of a positive coping strategy, peace of mind, and relaxation on your comfort and recovery. Studies have shown that patients who are prepared to experience pain after an injury or surgery tend to feel less pain and to feel more positive that their recovery is on track. The support of family and friends, as well as entertainment and laughter, can help during times of discomfort.
- Learn more: Alternative Methods to Help Manage Pain After Orthopaedic Surgery
- Discuss a pain relief plan with your orthopaedic surgeon and stick to it.
- Specify an appropriate plan to minimize pain, which may include a combination of opioids and other medications (this is called multi-modal pain management). Because some pain medications may have adverse (negative) effects when combined with even over-the-counter medicines or supplements, it is important to tell your doctor about all medications and supplements you are taking.
- Discuss how much pain is too much and how to know (in the rare instances) when a problem like an infection has occurred.
- If you are prescribed opioids, try to take them only when other alternatives are not working and stop taking them as soon as your pain begins to improve. Some strategies for taking less opioid medication include.
- Adding over-the-counter pain medications, such as acetaminophen (e.g., Tylenol) and ibuprofen (e.g., Advil) to opioid treatment. Before doing this, however, you should always check with your doctor. Many opioid pills already contain acetaminophen; in large doses, acetaminophen can cause serious side effects. In addition, people who are taking blood thinners should not take ibuprofen or any other nonsteroidal anti-inflammatory medications, such as naproxen (e.g., Aleve) or aspirin.
- If there is no acetaminophen in the opioid pills, add acetaminophen — either 2 extra strength pills every 6 hours around the clock or 2 regular-strength tablets every 4 hours around the clock for 2 days.
- Alternate the acetaminophen with ibuprofen so that you're taking one or the other every 3 hours, and never take more than 4 grams (4000 milligrams) of acetaminophen per 24-hour period.
- If you have had a nerve block (an anesthetic injection) that has worn off, you can take the stronger pain reliever every 3 hours for the next 3 doses.
- Take opioids only as prescribed.
- Never take more than instructed, take someone else's medicine, or give your medication to someone else.
- Never combine opioids with alcohol or anxiety medication.
- Never use opioids to treat anxiety or to sleep, out of fear of pain, or to feel good.
- Always store and dispose of opioids safely.
- Pain relievers are a leading cause of serious poisoning of children and pets when medications are left unsecured.
- Hide or lock up opioid medications to avoid access by family, friends, or houseguests.
- Keep prescription medications in their original packaging so it is clear for whom the medications were prescribed and the directions for appropriate use.
- Place unused opioids in a disposal unit in a hospital, pharmacy, or police station. To find a disposal site near you, visit the U.S. Drug Enforcement Administration's Controlled Substance Public Disposal Locations.
- AVOID too many doctors prescribing medication at once. Visiting multiple doctors to get multiple prescriptions for controlled substances like opioids is known as "doctor shopping." As medical record systems and state databases are implemented and improved, fewer patients will be able to secure pain prescriptions from multiple providers. And many states have already enacted laws along those lines.
In summary, while minimizing patient discomfort around surgery or an injury remains an important goal of orthopaedic care, great caution should be used in prescribing and taking opioids. Orthopaedic surgeons, and all physicians and health care professionals, are working together to change the culture of pain management in the U.S., with the goal of significantly reducing opioid use and misuse and saving lives.
Help Spread the Word
Share this information about prescription drug safety on your social media sites. Be sure to add #PrescriptionSafety to your posts.
Last Reviewed
May 2023
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.